"Biomedical lab in a box" empowers engineers in low- and middle-income countries
Globally, and especially in low- and middle-income countries (LMICs), a significant portion of the population lacks access to essential healthcare services. Although there are many contributing factors that create barriers to access, in many LMICs failing or obsolete equipment plays a significant role.
“Those of us who have investigated healthcare systems in LMICs are familiar with so-called ‘equipment graveyards,’” says Nevan Hanumara, SM ‘06, PhD ‘12, a research scientist in MIT’s Department of Mechanical Engineering, referencing piles of broken, imported equipment, often bearing stickers indicating their origins from donor organizations.
“Looking at the root causes of medical equipment failing and falling out of service in LMICs, we find that the local biomedical engineers truly can't do the maintenance, due to a cascade of challenges,” he says.
Among these challenges are: design weaknesses – systems designed for temperate, air-conditioned hospitals and stabilized power don’t fare well in areas with inconsistent power supply, dust, high heat and humidity, and continuous utilization; lack of supply chain – parts ordered in the US can arrive in days, where parts ordered to East Africa may take months; and limited access to knowledgeable professionals – outside of major metropolitan areas, biomedical engineers are scarce.
Hanumara, Leroy Sibanda SM’24, a recent graduate with a dual degree in Management and Electrical Engineering and Computer Science (EECS), and Anthony Pennes SB ’16, a technical instructor in EECS, began to ponder what could be changed if local biomedical engineers were actually involved with the design of the equipment that they’re charged with maintaining.
Pennes, who staffs 2.75/6.4861 (Medical Device Design), among other courses, developed hands-on biosensing and mechatronics exercises as class activities several years ago. Hanumara became interested in expanding that curriculum to produce something that could have a larger impact.
Working as a team, and with support from MIT International Science and Technology Initiatives (MISTI), MIT Jameel World Education Lab (J-WEL), and the Priscilla King Gray (PKG) Public Service Center, the trio created a hands-on course, exercises, and curriculum, supported by what they’ve now dubbed a “Biomed Lab in a Box" kit.
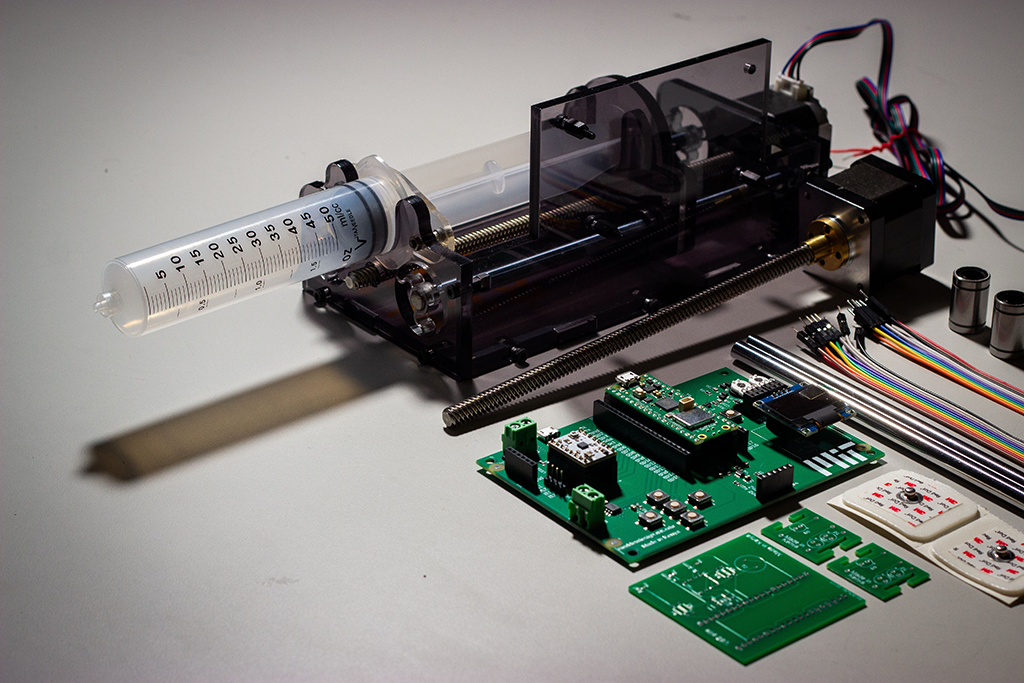 From top left to bottom right: Assembled syringe pump; Stepper motor with lead screw; Custom PCB with motor driver to control pump; Linear rails, wires, bearings; Additional PCBs for measuring ECG and pulse detection. Photo credit: Isabella Yu
From top left to bottom right: Assembled syringe pump; Stepper motor with lead screw; Custom PCB with motor driver to control pump; Linear rails, wires, bearings; Additional PCBs for measuring ECG and pulse detection. Photo credit: Isabella YuSibanda, who hails from Bulawayo, Zimbabwe, brings additional lived experience to the project. He says friends up and down the continent speak about great practical primary and secondary education, and a tertiary education that provides a heavy emphasis on theory. The consequence, he says, is a plethora of graduates who are absolutely brilliant at the theory, but less experienced in advanced practical concepts.
“Anyone who has ever had to build systems that need to stand up to real world conditions understands the chasm between knowing how to calculate the theoretically perfect ‘x’ and being capable of implementing a real-world solution with the materials available,” says Sibanda.
Hanumara and Sibanda travelled to Nairobi, Kenya, and Mbarara, Uganda, in late 2024 to test their kit and their theory, teaching three-day long biomedical innovation mini-courses at both Kenyatta University and Mbarara University of Science & Technology (MUST), with Pennes providing remote support from MIT’s campus.
With a curriculum based off of 2.75, labs were designed to connect the theoretical to the physical, increasing in complexity and confronting students with the real challenges of biomedical hardware and sensing, such as weak signals, ambient noise, motion artifacts, debugging, and precision assembly.
Pennes says the goal for the mini-courses was to shape the project around the real-world experiences of the region’s biomedical engineering students. “One of the problems that they experience in this region is not simply a lack of equipment, but the lack of ability to maintain it,” he says. “Some organization will come in and donate thousands of dollars of surgical lighting; then a power supply will burn out, and the organization will never come back to fix it.”
But that’s just the beginning of the problem, he adds. Engineers often find that the design isn’t open, and there’s no manual, making it impossible to find a circuit design for what’s inside the donated, proprietary system. “You have to poke and prod around the disassembled gear to see if you can discern the makers’ original goals in wiring it, and figure out a fix,” says Pennes.
In one example, he recalls seeing a donated screen for viewing x-rays – the lightbox kind used to backlight film so that technicians can read the image – with a burned-out bulb. “The screen is lit by a proprietary bulb, so when it burned out, they could not replace it,” he recounts.
Local biomedical engineers ultimately realized that they could take a number of off-the-shelf fluorescent bulbs and angle them to fit inside the box. “Then they sort of MacGuyver’d the wiring to make them all work. You get the medical technology to work however you can.”
It’s this hands-on, imaginative approach to problem-solving that the team hopes to promote – and it’s one that’s very familiar at MIT. “We’re not just ideas people, where we write a paper and we’re done with it – we want to see it applied,” says Hanumara. “It’s why so many start-ups come out of MIT.”
Course modules presented at Kenyatta and MUST included “Breadboarding an optical LED – photodetector pulse detector,” “Soldering a PCB and testing a 3-lead EKG,” and “Assembling and programming a syringe pump.” Each module is designed to be a self-contained learning experience, and the kit is accompanied by a USB flash drive with a 96-page lab manual written by Sibanda, and all the needed software, which is important to have when internet access is unreliable. The third exercise, relating to the syringe pump, is already available via open access from the journal Biomedical Engineering Education.
“Our mission was to expose eager, young biomedical engineers to the hands-on, Mens et Manus culture which is the cornerstone of MIT, and encourage them to develop their talents and aspirations as engineers and innovators,” says Hanumara. “We wanted to help empower them to participate in developing high quality, contextually appropriate, technologies that improve healthcare delivery in their own region.”
A LinkedIn post written by Hanumara, shared reflections from students on their experiences with the material. “Every lab—from pulse oximetry and EKGs to syringe pump prototyping—brought classroom concepts to life, showing me the real-world applications of what we study,” wrote Muthoni Muriithi, a student at Kenyatta University. “Using breadboards, coding microcontrollers, soldering components, and analyzing biological data in real-time helped me grasp how much careful design and precision go into creating reliable healthcare tools.”
Feedback provided by students at both institutions is already helping to inform updates to the materials and future pilot programs.
Sibanda says another key thing the team is tracking what happens beyond the sessions, after the instructors leave. “It’s not just about offering the resource,” he says. “It’s important to understand what students find to be the most valuable, especially on their own.”
Hanumara concurs. “[Pennes] designed the core board that we’re using to be multi-functional. We didn’t touch any of the functions he built in – we want to see what the students will do with them. We also want to see what they can do with the mental framework,” he says, adding that this approach is important to empower students to explore, invent, and eventually scale up their own ideas.
Further, the project addresses another challenge the team identified early on: supply chain issues. In keeping with the mission of local capacity building, the entire kit was assembled in Nairobi by Gearbox Europlacer, which operates the only automated circuit board line in East Africa and is licensed to produce Raspberry Pi’s microcontrollers. “We did not tell the students anything,” says Hanumara, “but left it to them to notice that their circuit boards and microcontrollers said ‘Made in Kenya.’”
“The insistence on local manufacturing keeps us from falling into the trap that so much equipment donated into East Africa creates – you have one of these items, and if some part of it breaks you can never replace it,” says Pennes. “Having locally-sourced items instead means that if you need another component, or devise an interesting side project, you have a shopping list and you can go get whatever you need.”
Building off our ‘Biomed Lab in a Box’ experiment,” says Hanumara, “we aim to work with our colleagues in East Africa to further explore what can be designed and built with the eager, young talent and capabilities in the region.”
Hanumara’s LinkedIn post also thanked collaborators, Professor June Madete and Dean Johnes Obungoloch (PhD), from Kenyatta and MUST, respectively, and Latiff Cherono, managing director of Gearbox. The team hopes to eventually release the whole course in open-source format.