Smart pill can track key biological markers in real-time
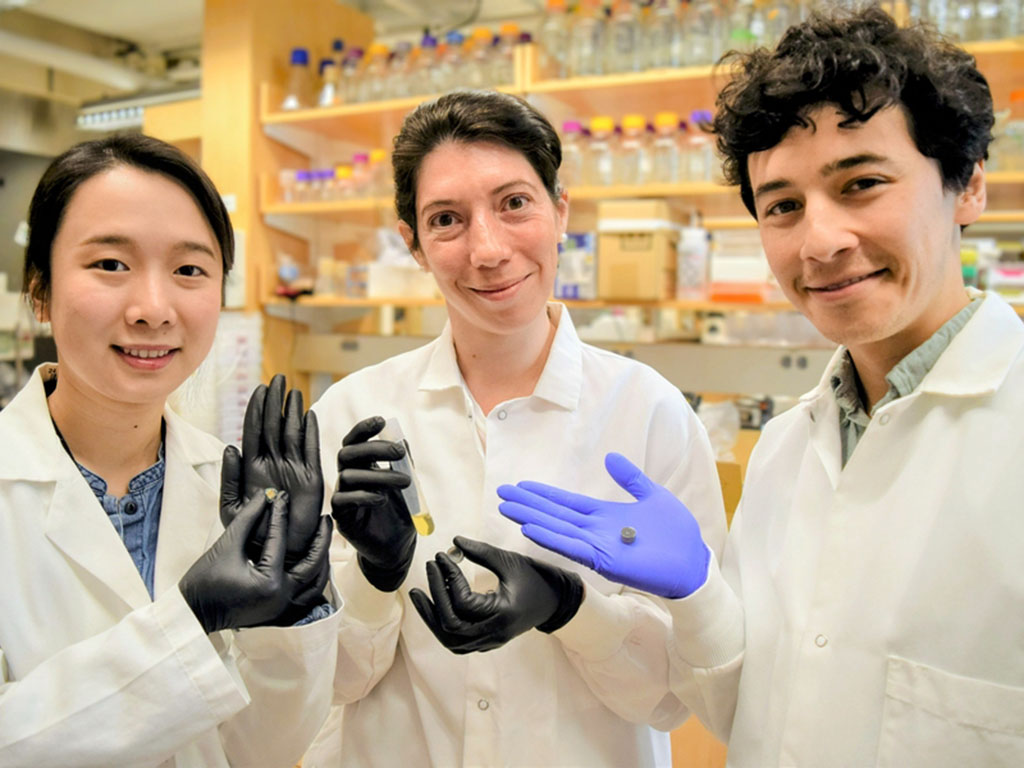
Researchers from MIT, Boston University, and elsewhere report a smart pill the size of a blueberry that could be a game changer in the diagnosis and treatment of bowel diseases. That’s because it is the first technology compatible with ingestion that can automatically detect — and report on in real time — key biological molecules that could be indicative of a problem.
The work appears in the Aug. 10 issue of the journal Nature. Other authors of the paper are researchers at Brigham and Women’s Hospital in Boston, the University of Chicago, and Analog Devices.
The new study significantly advances earlier research reported in a 2018 issue of Science. The current pill is approximately one-sixth the size of the prototype reported in Science, conforming to safe, ingestible dosage forms on the market. It has also been designed to detect key biological molecules, such as nitric oxide and byproducts of hydrogen sulfide, which are important signals and mediators of the inflammation associated with bowel diseases.
Current techniques for diagnosing diseases inside the gut can be invasive (think of a colonoscopy or other endoscopic procedure), and can’t detect molecular biomarkers of disease in real-time. The latter is a problem because several important biomarkers are very short-lived, so they disappear before current techniques can detect them.
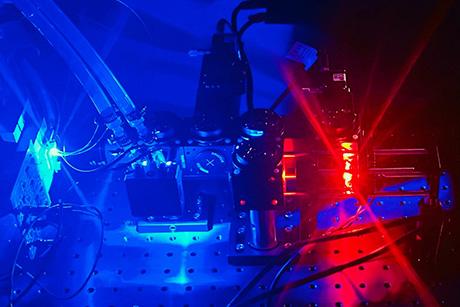
The new pill, which has been successfully tested in pigs, combines specially engineered living bacteria with electronics and a tiny battery. When the bacteria sense a molecule of interest, they produce light (the bacteria by themselves have also been successfully tested outside of animals and in mice). The pill electronics then convert that light into a wireless signal that can be transmitted through the body to a smartphone or other computer in real time as the pill travels through the gut.
“The inner workings of the human gut are still one of the final frontiers of science. Our new pill could unlock a wealth of information about the body’s function, its relationship with the environment, and the impact of disease and therapeutic interventions,” says Timothy Lu, an MIT associate professor of biological engineering and of electrical engineering and computer science. Lu, who is also affiliated with MIT’s Materials Research Laboratory and Senti Biosciences, is a senior author of the work described in Nature.
Potential impact
Roughly 7 million people around the world suffer from inflammatory bowel diseases (IBDs) like colitis or Crohn’s disease.
“One of the most challenging aspects of monitoring IBDs is the anticipation of clinical flares that often happen in these patients and that dictate pharmacological management of their diseases. At the moment we have no robust biomarkers that predict an upcoming inflammatory flare and, therefore, patients often experience severe symptoms that require hospitalization to be properly managed,” says Alessio Fassano, a professor at the Harvard T.H. Chan School of Public Health, who was not involved in the research. “This system may represent a game changer in the management of IBDs in terms of early diagnosis, interception of disease flareups, and optimization of a therapeutic plan.”
In their study, the researchers showed that the smart pill could detect nitric oxide, a short-lived molecule that is associated with many IBDs. Importantly, the sensors could also detect different concentrations of nitric oxide. “That will allow us to differentiate between a normal situation and disease,” says Maria Eugenia Inda, a Pew Postdoctoral Fellow in MIT’s Department of Electrical Engineering and Computer Science (EECS) and Department of Biological Engineering (BE). It’s also important because biomarker levels vary greatly among patients.
Understanding the gut
The team says the pill could be tweaked to detect other key biomarkers. As a result, Inda is also excited about the potential for the system to give scientists a much better understanding of the gut microbiome, or the delicate environment that harbors the microbes key to digesting food.
Currently, the gut is like a black box. “We still don’t fully understand it because it’s difficult to access and study. We lack the tools to explore it,” she says. “Knowing more about the gut chemical environment could help us prevent disease by identifying factors that cause inflammation before the inflammation takes over.”
Beyond the gut, the team’s combination of microbes and electronics could have broad use for health monitoring. “We played to the strengths of the biology and the electronics — our tiny pill shows what is possible when we can bridge bacterial sensing with wireless communication,” says Miguel Jimenez, a research scientist in MIT’s Department of Mechanical Engineering (MechE). Inda and Jimenez are co-first authors of the paper.
“Through this development we describe a unique platform for the evaluation of the GI tract which we anticipate can help many,” says Giovanni Traverso, an associate professor in MechE, a gastroenterologist at Brigham and Women’s Hospital, and one of the senior authors of the study.
A fantastic voyage
Inda compared the research to “Fantastic Voyage,” a 1966 film about four scientists who shrink themselves to fit into a tiny submarine that travels through the arteries of a sick man to treat a problem in his brain. “We scientists can’t do that,” she says with a smile, “but now we can send bacteria to do something similar. Rapid advances in synthetic biology are allowing us to harness the information-processing abilities of living cells to diagnose disease in such difficult-to-access environments.”
Inda, Jimenez, Traverso, and Lu’s coauthors of the Nature paper are Christoph Steiger, Alison Hayward, Adam Wentworth, and Wiam Madani of MechE, MIT’s Koch Institute for Integrative Cancer Research, and Brigham and Women’s Hospital (BWH); Nhi Phan and Jenna Ahn of the Koch Institute; Qijun Liu (who is also first author of a 2022 paper on the electronics), Arslan Riaz, Timur Zirtiloglu, and Rabia Yazicigil of Boston University Electrical and Computer Engineering Department; Kaitlyn Wong and Ronan McNally of BWH; Keiko Ishida of the Koch Institute and BWH; Niora Fabian of MechE, the Koch Institute, and MIT’s Division of Comparative Medicine (DCM); Josh Jenkins and Johannes Kuosmanen of MechE and the Koch Institute; Yong Lai of BE and EECS; Alison Hayward of MechE, the Koch Institute, BWH, and DCM; Mark Mimee of the University of Chicago; Phillip Nadeau of Analog Devices; and MIT Dean of Engineering Anantha Chandrakasan, a professor of EECS.
This work was supported by the Leona M. and Harry B. Helmsley Charitable Trust, the Pew Charitable Trusts, the Translational Research Institute of Space Health, the MIT Department of Mechanical Engineering, the MIT Karl van Tassel (1925) Career Development Professorship, and the Catalyst Foundation.